The Guide to Eczema Causes, Atopic Eczema, and Triggers for Atopic Dermatitis
1. What skin condition causes itchy rashes and dermatitis?
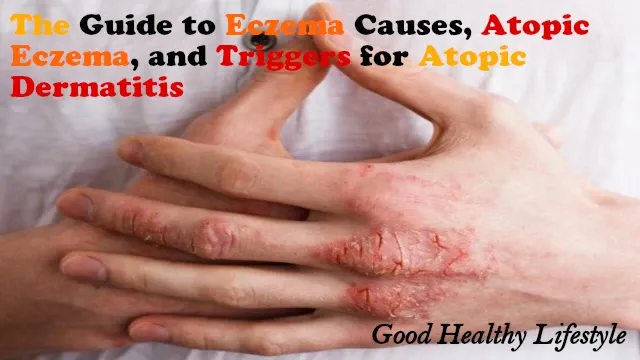
For many folks, an ongoing battle with irritating dry, itchy skin patches is just part of life. The condition causing these symptoms is commonly known as eczema. Both children and adults can develop eczema, an inflammation of the skin that leaves it red and flaky. The itch is often relentless, particularly at night, and folks frequently wake to find they've inflicted skin infections from scratching too much during flare-ups. Nummular eczema causes coin-shaped rashes while dyshidrotic eczema buds tiny fluid-filled bumps. Managing eczema is key, as triggers like soaps, sudden weather changes, or stressful periods can make symptoms worse quickly. Moisturizing daily with cream, limiting fragrant laundry products, and bathing in lukewarm water help eczema sufferers prevent flares of their chronic skin disease. Seeing a dermatologist allows them to create a tailored treatment plan utilizing topical steroids or light therapy to reduce itch and inflammation. Proper eczema care is crucial for comfort.
2. What are the main symptoms of eczema flare-ups?
That pesky eczema can really flare up at inopportune times, let's tell you. The main symptoms folks see are inflamed skin that causes the skin to become itchy as hell. Rashes from eczema tend to erupt in typical spots like the backs of the knees, inner elbows, and lower legs. Sometimes the skin just looks red and scaly, other times it blisters and weeps. triggers like soaps, fabrics, and stress to compromise the skin barrier and bring on eczema rashes. I remember one kid who had such bad flare-ups every winter, it was like he took a dip in a pool of calamine lotion daily to find some relief!
In addition to the itch and rough appearance, flare-ups make people susceptible to skin infections too if the inflamed skin is left unaddressed. That's why experts recommend usin' over-the-counter topical creams containin' hydrocortisone or prescription ointments if the rash is especially weepy or widespread. Soothin' that cranky skin and fixin' the barrier is key to preventin' further irritation and risks of skin infections. Folks should talk to a dermatologist if flare-ups are frequent or severe, as new prescription treatments for eczema skin disease may help better control this troublesome skin condition long term.
3. What eczema triggers should be avoided to help prevent eczema symptoms?
Certain fabrics, soaps, and detergents are notoriously irritating for individuals diagnosed with eczema, often triggering itchy, dry, and inflamed skin patches. Symptoms frequently flare when people with sensitive skin types use harsh cleaning products or wear materials like wool and lycra that don't allow the skin to breathe easily. The National Eczema Association recommends choosing gentle fabrics like cotton and bathing with fragrance-free cleansers to better manage moderate to severe eczema. Stress is another classic trigger, as cortisol levels spike and weaken the skin barrier that helps prevent dry skin. For children who may develop the form of eczema known as atopic dermatitis, potential triggers include pet dander, dust mites, and indoor allergens as well as changes in temperature. It is important for patients to identify personal triggers, as various foods, chemicals, or environmental allergens can induce eczema symptoms in some cases.
Developing a treatment plan in consultation with a dermatologist helps tailor topical treatment options to an individual's unique presentation of this chronic skin disease. This includes learning to manage stress, wearing loose, breathable clothing, keeping the home clean, and regulating indoor climate as prevention techniques. With awareness and avoidance of triggers, many eczema sufferers see an improvement in their chronic condition. However, flare-ups may still occur, so using prescribed creams is important to treat inflammation swiftly and curb worsening symptoms. It just takes persistent management and treatment.
4. What is the most common type of eczema seen in children?
The most common type of eczema seen in children is atopic dermatitis, otherwise known as child eczema. Child eczema is a chronic skin condition that causes dry, itchy skin and rashes. Infants and children with child eczema often have patches of extra dry, rough, and scaly skin on the cheeks, arms, and legs. The dry skin is due to inherited problems with the skin's natural protective layer that allows moisture to rapidly escape from the surface of the skin.
The symptoms of child eczema are itchy red rashes that often worsen due to things that trigger eczema, like contact with wool, soap, dust mites, food allergies, and sensitive skin products. Creams and ointments containing hydrocortisone help reduce inflammation and ease symptoms. A good skincare routine is important for mild to moderate cases to avoid things that cause the skin to dry out or become irritated. Keeping skin well moisturized is also key to managing symptoms. Most children will outgrow their child eczema before adulthood as their immune system matures. However, some may continue having outbreaks of eczema into adulthood, requiring ongoing treatment. With proper treatment and management, many people are able to control their symptoms effectively.
5. What are the symptoms of atopic eczema that affect children?
The most common signs of child eczema in children are itchy, dry patches of skin. Kiddos with this type of eczema regularly get irritating red rashes behind the knees and inner elbows that just wanna be scratched constantly, but you gotta resist that urge! The itch is usually worse at night too, poor things.
Another frequent sign is tiny blisters filled with clear fluid, known as vesicles, showing up on the hands and feet. These pixelated patches are super uncomfortable no doubt. Facial eczema around the eyes and cheeks is also pretty typical. The skin becomes scaly, leathery, and maybe even cracked - ouchie! It can act up from things like soapy baths, wooly clothes, or stress. Thankfully most children will outgrow their eczema as they become teenagers.
In the meantime, moisturizing daily with medication prescribed by the doctor helps keep scales soft and itchin' managed. Anti-itch pills and avoiding known triggers are also key to preventing uncomfortable breakouts. With some TLC routines, most kiddos can still enjoy playtime without too much bother from their irrational skin. Fingers crossed modern medicines continue findin' new ways to help these itty bitty patients feel more comfy in their own flesh.
6. What are the external factors to cause eczema rash, and is it contagious?
There are numerous external factors that can induce an eczema outbreak in both children and adults. Common provocations include soaps, fabrics like wool, and excessive heat or dryness that disrupts the skin's natural protective layer. Stress is another significant factor - when cortisol levels rise, it makes irritated skin even more bothersome.
Certain foods are also culprits for some people with atopical dermatitis. Dairy, eggs, peanuts, and shellfish are frequent causes of food sensitivities in people with eczema. When an irritant is touched or ingested, it sets off a chain reaction in the body that results in reddened, itchy patches of dermis on the hands, feet, or lower legs. Those with a history of eczema are more prone to developing other inflammatory covering conditions such as hay fever or contact allergy.
Identifying one's unique exacerbating elements takes experimentation. Keeping a diary of potential aggravating factors can help people diagnosed with eczema recognize patterns and exposures that cause their signs and symptoms to flare up. It’s important to maintain a regular skincare regimen with frequent application of a moisturizing treatment and avoid harsh soaps, allowing the skin's protective barrier to stay intact. With proper long-term management of breakouts, many find their eczema is mild to moderate and controllable when the causes are treated. Continued topical treatments and regimens tailored to the individual can lead to relief of uncomfortable eczema indications.
7. What treatments are used to manage eczema flare-ups and symptoms of atopic dermatitis?
There are several options for treating episodes of worsening inflammation and signs of atopic dermatitis. Moisturizers are critical for skin care since dry, itchy skin is a major trigger for flare-ups. I always have an unscented moisturizer on hand to apply after baths while my skin is still damp - this helps lock in moisture and prevent further drying of affected skin areas. Ointments work even better than lotions for me on really dry areas of skin. When my dermatitis causes only mild irritation, these basic skin care steps usually do the trick. But lately, with this nasty winter weather, my condition has seemed to worsen, with inflamed, scaly areas appearing on my hands and forearms. Steroid ointments are very effective for bringing down inflammation when I feel the condition worsening. They can cause side effects with long-term use, so I only apply them when irritated skin areas are more severe.
For people with atopic dermatitis, additional treatment options may involve prescription medications aimed at modifying the immune system response and reducing inflammation. Immunosuppressants can provide relief for cases where basic moisturization and topical steroids prove insufficient on their own. Contact dermatitis can also affect different areas of the body and skin may become rough and flaky. Phototherapy is another alternative sometimes used - it involves controlled exposure to specific wavelengths of ultraviolet light that may help recalibrate overreactive skin cells. I read new biological drugs targeting precise elements of the immune pathway show promise too. Finally, complementary approaches like aromatherapy, stress management techniques, and consideration of potential allergens that could impact the dermatitis may offer supplemental relief for many patients. The most effective treatment regime will likely involve trial and refinement to determine the best regimen for controlling individual signs long-term.
8. What are the relative strengths and limitations of medical eczema treatments vs. natural cures for eczema?
Both medical treatments and natural cures have their strengths and limitations for managing eczema. Prescription ointments and gels effectively relieve itching and reduce inflammation during flare-ups. However, they are not a long-term cure and often require continuous use. Natural remedies like intensive moisturizing and identifying aggravating foods offer a gentler long-haul approach, but patchy skin and rashes may still arise occasionally as symptoms take time to subside.
Layering modalities seem most effective. Prescription corticosteroids provide hasty relief for severe flares. Then, moisturizing balms hydrate dry, irritated skin while antihistamines help symptoms exacerbated by hay fever. Identifying personally-activating foods like tomatoes and dairy and avoiding intake supports self-care minus sole dependence on medications. Determining the optimal plan involves testing prescribed gels with natural balms during episodes or assessing dietary provocateurs. Adapting cures to the individual realizes the best control over eczema symptoms. Productive dialog between clinicians and patients helps establish the right modulated solution. Treating inflammation appropriately and reducing mild to moderate eczema long-term depends on disciplined skincare and sticking to suitable eczema treatments.
9. How should management and treatments for eczema in children change and adapt over time as kids' ages and needs differ?
Managing dermatitis in children requires customized tactics as needs change throughout development. What soothes an infant's dry, irritated skin may not effectively help elementary-aged children handling moderate to severe atopic or contact dermatitis along with associated allergic rhinitis. Healthcare providers must partner with caregivers to develop individualized plans tailored to each developmental stage. For babies, identifying moisturizing cleansers, emollients, and fabrics that don't exacerbate blotchy skin patches across different areas of the body is key to reinforcing compromised barriers. Testing various moisturizers, oatmeal-infused skin care routines, and cotton sleepwear can relieve sore joints and prevent infected patches or other complications affecting highly irritated regions.
As children with eczema enter preschool, consistent modification as part of a daily skin care regimen helps keep inflamed surfaces hydrated and limits exacerbations from irritants like allergens, pollen, or fungi exacerbating signs and symptoms. Topical corticosteroids and oral antihistamines provide overnight relief from relentless itching and swelling. By pre-teens and teenagers, finding stress relief through favorite activities rather than scratching treated cases prevents worsening discoid eczema. Comprehensive allergy screening aids in identifying specific food allergies fueling weekly symptom severity. Throughout childhood, medical providers and parents must collaborate to customize care plans, including approaches to treat eczema, tailored to the child's evolving needs as dermatitis is a chronic condition negatively impacting many into adulthood if improperly managed during each developmental stage.
10. How do genetics and family histories relate to repeating patterns of symptoms and causes of atopic eczema?
Research shows that eczema is often hereditary. When individuals have a family history of dealing with dry, itchy patches since childhood, they are more likely to develop signs of eczema themselves over time. Studies find that exacerbations of eczema frequently affect the same body areas in family members, suggesting a genetic component influences manifestation patterns. Carrying genes that make the outermost skin layer highly sensitive to irritants or provoke an over-reactive immune response could explain this trend. A diagnosis of atopic dermatitis, a long-term condition, means carefully managing inflammation and devising strategies to stave off worsening eczema.
Scientists continue exploring how genetics contributes to eczema persistence. Some hypotheses point to inherited factors potentially impacting the skin’s protective barriers or immunity deregulation, both of which can induce worsening episodes of eczema. This may account for familial tendencies like very dry, easily aggravated skin prone to outbreaks from minor provocations. Designing personalized skincare approaches addressing specific exacerbating influences, such as certain cleansers or allergens, helps monitor eczema. While a cure remains elusive, adhering to a consistent moisture-based skin care routine is key to avoiding the severe, infected types of eczema patients have struggled with for extended periods due to genetic vulnerabilities. Proper hydration aids in preventing eczema progression past mild or moderate stages. Inherited weaknesses could make individuals prone to developing different forms of eczema like discoid eczema or infected eczema over their lifetime.
11. What environmental and dietary triggers can cause of eczema flares in sensitive individuals?
Certain environmental conditions can cause eczema gushes in many people who have reactive skin. Folks with contact dermatitis really struggle when exposed to irritants like harsh soaps, wool fabrics, or chemicals. People with nummular eczema tend to see their patches of skin on the legs or torso get worse too. Exposure to allergens like pet dander or dust mites is a common symptom provoker for kids with atopic dermatitis. Some notice certain foods will send their eczema into a tailspin as well. Dairy, tomatoes, and nuts are frequent food activators that need to be avoided. Keeping a food diary can help identify the dietary culprits causing their symptoms to flare.
Moisturizing daily is key for managing dry skin, which is a trademark symptom for many adults with eczema. Using a thick ointment or balm right after bathing helps strengthen the epidermis and prevent inflammation. Stress is another significant provoker that can induce a flare for folks with seborrheic dermatitis on the scalp. Developing a strategy with their dermatologist is important for getting long-term control. Those with moderate to severe cases may need prescription medications to better manage their symptoms between flare-ups. Simple lifestyle changes, moisturizing religiously, and following their strategy can help many children outgrow their eczema as they get older.
12. Which activities or occupations seem to be most impacted when eczema affects certain body areas?
For many individuals dealing with contact dermatitis or dyshidrotic eczema, flare-ups in specific regions can seriously interfere with occupations. Jobs requiring extensive use of the palms of the hands or regions of skin between fingers tend to be most impacted, as cracked, irritated skin causes discomfort worse and makes tasks painful to perform. Musicians, for example, may struggle greatly when patches develop on areas they need for fingering instruments skillfully. Even simple actions like driving can prove difficult, as repeated contact and motion exacerbate symptoms. Those with various types of eczema like atopic dermatitis or seborrheic dermatitis that cause dry, scratchy skin can also have their hobbies disrupted. Gardeners and cooks often find their interests affected when flares emerge on forearms, as favorite pastimes involve the inflamed region. Managing eczema signs during leisure pursuits can feel discouraging.
The influence fluctuates depending on the localization and severity of eczema. Those with moderate to severe cases leading to the skin condition that causes dry, cracked skin have a more prominent impact on lifestyle. Occupations requiring manual dexterity may require treatment changes to accommodate eczema or medical leave. Hobbies commonly rely on affected areas for discomfort too. Proper treatment and preventative measures under guidance from a dermatologist can help reduce the duration and frequency of interference. This aids in undertaking work and enjoyable activities despite eczema, a chronic condition. With care and management of symptoms, quality of life need not suffer greatly even for adults with eczema.
13. How might novel eczema diagnosis techniques aid in evaluating less understood eczema causes like fungal or bacterial involvement?
Novel diagnostic techniques could help uncover less understood causes of eczema like fungal or bacterial motivations. While the root reasons for eczema ain't always clear, modern methods may shine a light on culprits beyond the usual suspects of genetics or environmental allergies. Being able to better diagnose the irritant for somebody's extreme eczema would be huge - it could lead to more targeted treatment programs bust some stubborn cases that don't seem to clear up otherwise.
One such promising technique is the microscopic examination of skin samples using state-of-the-art digital pathology. Unlike traditional skin scraping under the microscope, digital pathology allows for magnifying skin cells and structures up to a cellular level. This level of detail might spot fungal spores or bacterial overgrowth invisible to the naked eye. If symptoms are seen in the skin that looks infectious, they can prescribe an anti-fungal or antibiotic to get rid of it. With the right treatment, the inflammation and itch from dermatitis could calm down where nothing else has worked. Only time will tell if these sophisticated diagnostic methods start yielding more answers, but it sure would be nice to give folks new hope for managing their miserable areas of skin.
Currently, people with atopic dermatitis have limited options when other therapies for eczema flares fail. Advanced diagnostics exploring previously overlooked causes like fungus or bacterial involvement could lead to more effective solutions. Even identifying motivation factors would help individuals develop a treatment program and manage symptoms of eczema including itching, dryness, inflammation, and irritation. With more targeted strategies to prevent flares that disrupt daily lives, people with severe eczema may see an improved quality of life.